Introduction
An uncommon benign lesion called hepatocellular adenoma is most frequently observed in young women who have used oral contraceptives in the past. Although many lesions have been observed, it is usually solitary.
Hepatocellular adenomas often show regions of hemorrhage and infarction upon physical inspection, and pathologic study typically reveals a well-circumscribed, non-lobulated lesion.
Today, the main emphasis is on prevention, even if the gastroenterologist and the surgeon are the major providers of interprofessional care for the illness. In terms of patient education, both the pharmacist and the nurse are essential. Better patient outcomes will come from interprofessional treatment. So here is an elaborated discussion about “hepatic adenoma radiology”
What is hepatic adenoma Radiology?
Hepatic refers to the liver and adenoma refers to benign tumor. Collectively called Benign liver lesions that have been connected to oral contraceptives and anabolic steroids. Women who are on the pill and of reproductive age account for the bulk of these lesions. The lesions are benign, although bleeding and malignant change are possible outcomes.
Radiology refers to the technology that is responsible for imaging the internal organs to diagnose or treat the disorder.
Hepatic radiology: what is it?
A radioactive substance is used in a liver scan to evaluate liver masses and any deformity present in it and determine how effectively the liver or spleen is functioning.

Diagnosis
Patients with hepatic adenomatosis and glycogen storage disorder are more likely to develop several lesions such as GIT lesions or various tumors. Prompt diagnosis and treatment of hepatocellular adenomas is important due to the potential for bleeding and malignant change.
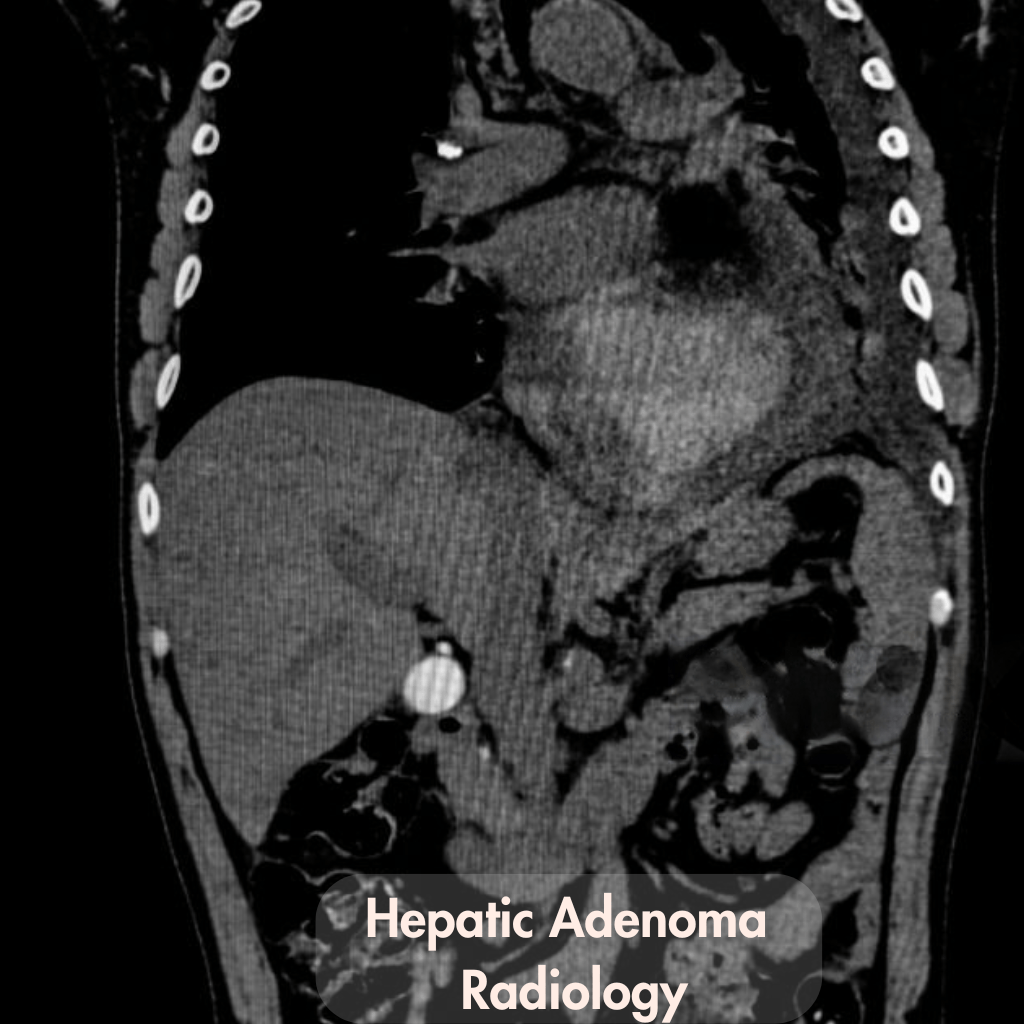
The majority of adenomas are often subsequently assessed using computed tomography (CT) or other imaging modalities because ultrasonography (US) is not always used to diagnose them precisely.
Hepatica adenomatosis
The existence of several hepatic adenomas, exceeding 10 and reaching up to 50, is known as hepatic adenomatosis. It is an uncommon condition that an MRI can best describe.
Epidemiology
Studies indicate a shift from the generally reported female predominance linked to the use of oral contraceptives to an increased prevalence in men, specifically acknowledging that obesity and metabolic syndrome are emerging risk factors for adenomas. but it is not true all the time.so, The incidence of hepatic adenomas is unknown.
Typically, the most common hepatic tumor in young women has been identified as hepatic adenoma;
- using the oral contraceptive pill
- having glycogen storage deformity
- having diabetes
- or using anabolic steroids frequently
Prognosis and treatment
Generally speaking, adenomas are removed when practical to definitively confirm the diagnosis and reduce the possibility of a spontaneous rupture as it can cause further lesions. Magnetic resonance Imaging is used to monitor lesion size and serum alpha-fetoprotein (AFP) levels when the lesion is small, not subcapsular, and seems normal.
Additionally, oral contraceptives are stopped if the patient has diabetes then it should be controlled; in these cases, the adenoma may regress. Hepatic arterial embolization may be useful in patients who are not treatable.
Case representation
Patient Data Presentation
Gender: Female Abdominal pain on the right side
Age: 40 years old
Once came a case of an American lady whose primary care physician recommended her to an internal medicine consultation to rule out a secondary cause of hypertension. Ten years prior, the patient was prescribed
- losartan 50 mg intravenously,
- hydrochlorothiazide 12.5 mg intravenously,
- atorvastatin 20 mg intravenously
for the treatment of mixed dyslipidemia and hypertension.
Pt. history

The patient’s lipid profile was normal, but her hypertension was not well managed. She had been under combined OCP for the previous 17 years and had a history of 13 pack years of smoking. There was no additional pertinent personal or family history other than this. She denied using recreational drugs or taking any over-the-counter medications.
Diagnosis
Her physical examination revealed no unusual findings for temperature or blood pressure, and she had no symptoms.
Risk factors for HCA complications – rupture and bleeding, and malignant transformation
| Rupture and bleeding | Malignant transformation |
| Diameter of 5 cm or more Sonic hedgehog HCA Arteries within the lesion Location in the left lateral liver Exophytic growth Pregnancy | Diameter of 5 cm or more ẞ-Catenin expression Male sex Glycogen storage disease Hormone consumption. |
Measures taken
A multidisciplinary team reviewed and presented the case; given the minimal risk of sequelae, such as hemorrhage, malignant transformation, or adenoma rupture, a cautious approach was taken, with biannual laboratory and imaging follow-up.
She stopped using OCP and had tubal ligation as a form of contraception. The quantity and size of nodules did not change six months following the diagnosis and stopping OCP, however laboratory markers of inflammation and AP gradually returned to normal levels.
After receiving
- perindopril 10 mg,
- bisoprolol 5 mg,
- amlodipine 5 mg,
- and atorvastatin 20 mg
once daily for the treatment of arterial hypertension and dyslipidemia, the patient is doing well and exhibiting no symptoms a year after the diagnosis.
laboratory results during the initial visit and subsequent visits.
| 1st appoint- ment | 6 months after stopping OCP | |
| Hb, g/dL (12-16) | 12.6 | 13.3 |
| Leukocytes, × 103/UL (4-10) | 12 | 9 |
| ESR, mm/1st h (<12) | 26 | 12 |
| INR (<1.3) | 0.87 | 0.89 |
| ALT, U/L (<70) | 22 | 14 |
| AST, U/L (<45) | 22 | 18 |
| AP, U/L (40-150) | 189 | 152 |
| GGT, U/L (12-58) | 48 | 47 |
| BrbT, mg/dL (<1.29) | 0.26 | 0.8 |
| Albumin, g/L (39-51) | 45 | 44 |
| CPR, mg/dL (<0.8) | 2.6 | 0.9 |
| AFP, ng/mL (<8.6) | _ | 1.6 |
Note: The reason for this case’s “heritage” designation is that it no longer complies with image processing and/or other case publishing requirements.
Magnetic Resonance Imaging(MRI)
A diagnostic examination called magnetic resonance imaging (MRI) may produce highly detailed pictures of almost every organ and structure inside the body. MRI creates pictures on a computer by using radio waves and magnets. Ionizing radiation is not used in MRI scans. An MRI scan can create images that display blood arteries, muscles, bones, and organs like the liver and brain.

MRI of the liver shows two types of appearances:
- Expansive appearance:
Because there is usually a lot of fat and no bile present, the lesion is well-circumscribed, clear, typically subcapsular, and yellow in color. Hemorrhagic shift happens often. A fibrous pseudo capsule may surround the tumor. - Tiny appearance:
Pleomorphic hepatocytes proliferate in hepatic adenomas without typical lobular architecture, according to histology. These cells often contain large amounts of glycogen, which explains the connection to von Gierke’s illness. They are commonly thought to be lacking in Kupffer cells and bile ducts, yet research has revealed that this is not always the case and that Kupffer cells are often reduced in numbers 1, 3, and 4. Tc-99m sulfur colloid scans are significantly affected by this.
MRI Results and HCA Subtype Clinical Characteristics
| Clinical features and MRI sequence | I-HCA | H-HCA | β‐HCA | U-HCA |
| T1 weighted imaging | From isointense to slightly hyperintense | From Isointense to hyperintense | From Isointense to hyperintense | No particular findings are known. |
| T2 weighted imaging | Significantly Hyperintense T2 Atoll sign: Incomplete T2 hyperintense rim | From isointense to slightly hyperintense | T2 hyperintense scar poorly defined | |
| Post‐contrast imaging | vascular enlargement that continues into subsequent stages. | varying arterial enlargement that disappears in subsequent stages | may have arterial augmentation and discharge to resemble HCC. the ill-defined scar that becomes better throughout the portal venous phase During the hepatobiliary phase isointense or hyperintense | |
| Imaging both in-phase and out-of-phase | There can be a small focused signal loss. | Substantial signal loss in photos that are out of phase. | Typically, there is no signal loss | |
| Rate of prevalence | Between 40%‐50% of cases | Between 30%‐40% of cases | Between 15%‐20% of cases | 10% |
| Possibility of malignant transformation | 11% | minimal danger As much as 46% 8 14% 13 Bleeding16%–30% 12, 13 % 12, 13, | As much as 46% | 14% |
| Bleeding | Between 16%-30% | About 9% | 14% | Between 14%-33% |
| Management factors | if less than 5 cm and steady, use cautious management. | If less than 5 cm and steady, use cautious management | Removal of tissue regardless of size; | conservative treatment if less than 5 cm and stable |
Here used abbreviations are:
| β‐HCA (β‐catenin‐mutated hepatocellular adenoma) HCA ( hepatocellular adenoma) HCC (hepatocellular carcinoma) H‐HCA (hepatocyte nuclear factor‐1‐alpha–mutated hepatocellular adenoma) HNF‐1α (hepatocyte nuclear factor‐1‐alpha) | L‐FABP ( liver fatty acid binding protein) MRI (magnetic resonance imaging) OATP1B3 ( organic anion transporting polypeptide ) U‐HCA (unclassified hepatocellular adenoma) I‐HCA (inflammatory hepatocellular adenoma) |
Conclusion of Hepatic Adenoma Radiology
Because of its rarity and lack of complete understanding of its physiopathology, treatment, and strategy, hepatic adenoma is a therapeutic challenge. In the majority of instances, an excisional biopsy is necessary for an accurate diagnosis so that it is treated in a good manner otherwise the condition can be worse.
Preventing its consequences is vital, and each patient should have a customized treatment plan prescribed by his physician, which has recently changed due to the discovery of molecular subtypes as different subtype has different consequences.
FAQs
How is hepatic adenomatosis treated?
Most cancers are amenable to local resection or segmental partial lobectomy i.e. defected lobe removal. Resection of the biggest lesions might prove to be the best course of action in situations of numerous hepatic adenomas.
How does hepatic adenoma appear clinically?
Patients with hepatocellular adenomas (HCAs), also known as hepatic adenomas, may have nonspecific physical examination findings. Patients may exhibit yellowing and stomach trouble, or they may show no symptoms at all.
how can I distinguish an HCC from an adenoma?
You can differentiate HCC from HCA by determining the type of tumor.
HCC are common, malignant tumors that often occur in a hemorrhaging background as the tumor is not localised.
HCAare benign tumors that are localized resulting from the overgrowth of hepatocytes in a liver showing no abnormality.
What characteristics does an ultrasound show for a hepatic adenoma?
Commonly there are three basic ultrasound features.
Simple adenoma is represented by hypoechoic, hyperechoic adenoma represents fatty metamorphism, and hemorrhagic necrosis is demonstrated by mixed-echoic patterns in tumors.
Is hepatic adenoma always symptomatic?
No, hepatic adenomas can be asymptomatic and incidentally discovered during imaging studies performed for